Explore All Articles
Explore All Articles

Coenzyme Q10 (CoQ10) is a fat-soluble, vitamin-like molecule found in nearly every cell of the body. Your heart depends on it more than most organs because it must generate energy continuously, without rest, for an entire lifetime.
This article explains what CoQ10 does, why it matters for heart health, and how to interpret the scientific evidence without oversimplifying or overstating it.
Medical note: This article is for educational purposes and is not a substitute for medical care. If you have heart disease or take prescription medications, discuss any supplement use with a qualified healthcare professional.
What keeps your heart beating more than 100,000 times a day without running out of fuel?
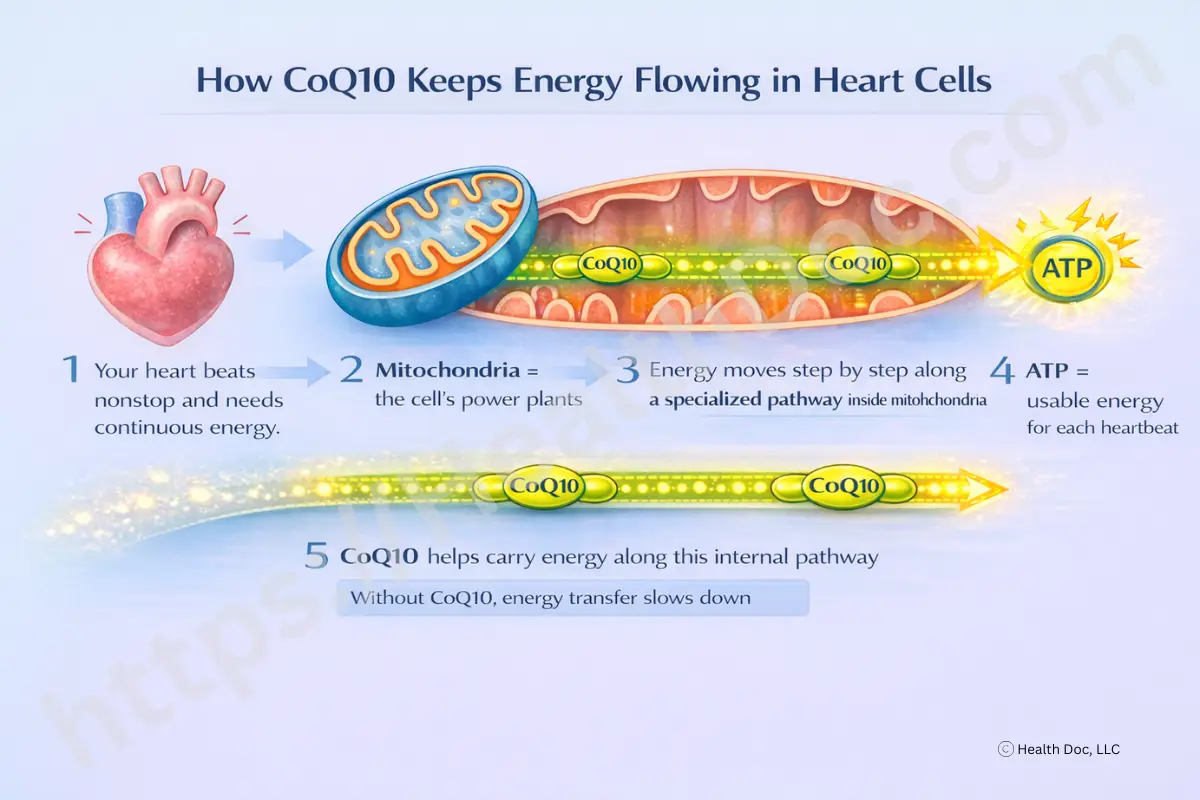
The short answer is ATP, or adenosine triphosphate. ATP is the molecule your cells use to store and spend energy. Every time your heart muscle contracts, it burns ATP - and it has to immediately replace it.
ATP is made inside mitochondria, often described as the “power plants” of the cell. Coenzyme Q10 is a fat-soluble, vitamin-like molecule that lives inside these mitochondria and helps them do their job.
CoQ10’s importance to the heart isn’t abstract. The heart cannot slow down, rest, or switch to a lower-energy mode for long. That makes it especially sensitive to anything that interferes with mitochondrial energy production.
Why does heart muscle contain so many mitochondria compared with other tissues?
Most cells can tolerate fluctuations in energy demand. Heart cells cannot. They contract continuously, day and night, for decades.
Because of this:
When mitochondria struggle, the heart has less energy available for each beat, and oxidative stress - the buildup of reactive byproducts of metabolism - tends to increase.
So where does CoQ10 actually fit into this process?
Inside mitochondria, ATP is produced through a sequence of chemical reactions called the electron transport chain. CoQ10 acts as an electron carrier, meaning it helps move electrons from one step to the next.
You can think of it like a relay runner. The race doesn’t work if one runner drops the baton. When CoQ10 levels are low or its function is impaired, the handoff becomes less efficient:
This dual role - supporting energy production while limiting oxidative damage - is why CoQ10 attracts interest in heart health.
When people say “antioxidant,” should you be skeptical?
Cautiously skeptical - but informed.
Oxidative stress occurs when reactive oxygen species (“free radicals”) outpace the body’s antioxidant defenses. These molecules aren’t villains; they’re normal byproducts of oxygen metabolism. But in excess, they damage lipids, proteins, and DNA.
CoQ10 is unusual because it plays dual roles:
This is especially relevant for lipid peroxidation, a process that damages cell membranes and mitochondrial machinery - like rancidity developing in cooking oil.
Do people with heart failure actually have lower CoQ10 levels - and should that concern you?
Observational studies consistently show that people with chronic heart failure tend to have lower circulating CoQ10 levels than people without heart failure. More importantly, one large cohort study found that lower plasma CoQ10 levels were associated with a higher risk of death, even after accounting for age, kidney function, and established heart-failure markers.
What does this mean in practical terms?
It does not prove that low CoQ10 causes heart failure or that supplementation will reverse it. But it does suggest that CoQ10 status reflects something meaningful about the metabolic health of the failing heart.
This is why CoQ10 has been studied as a supportive, add-on strategy, not as a replacement for standard medical treatment.
For readers who want deeper clinical context, see:
👉 CoQ10 and Heart Failure
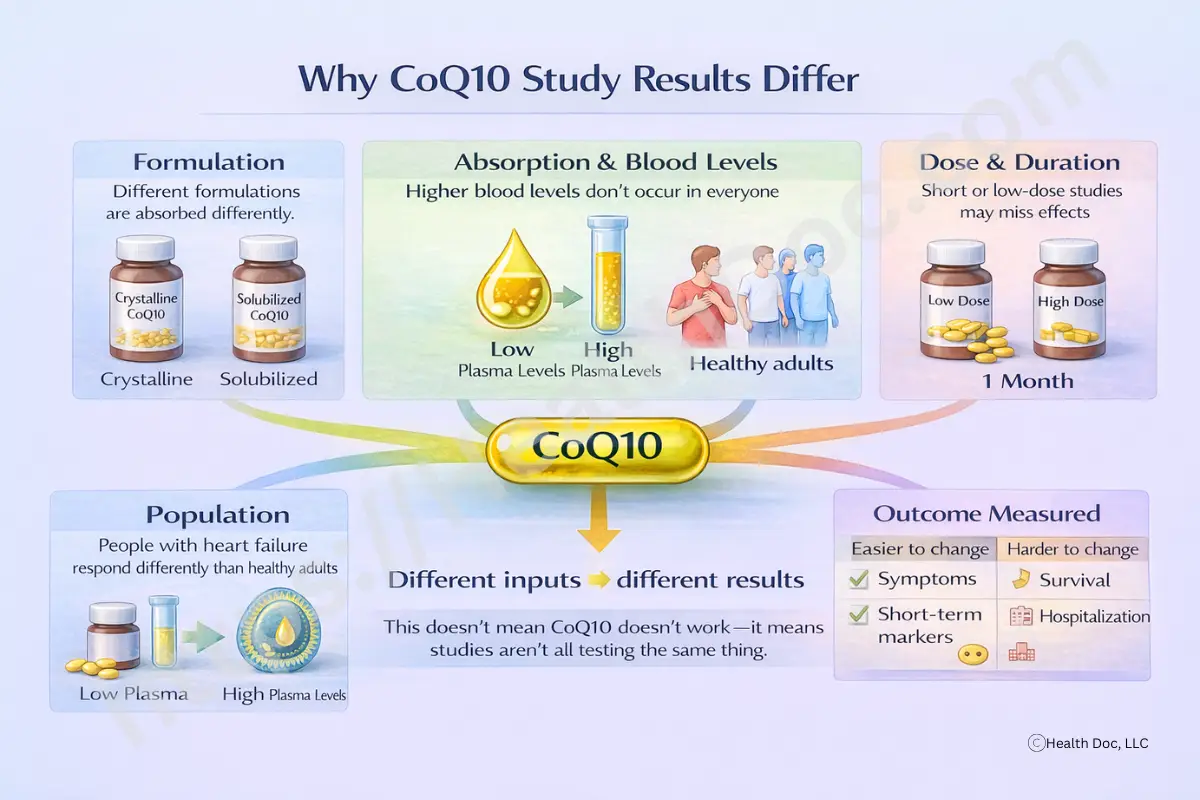
If the biology makes sense, why don’t all studies show the same benefits?
Because real-world research is messy.
When researchers combine multiple CoQ10 trials into meta-analyses, they often report heterogeneity. In plain language, this means:
Researchers also note that the overall certainty of evidence is often low to moderate, not because studies are useless, but because:
You may also see mention of publication bias, particularly for metabolic outcomes like blood sugar or cholesterol. This means studies with positive results are more likely to be published than studies showing no effect. For readers, this matters because it means the literature can look more optimistic than real-world results justify.
In short: inconsistent results don’t mean CoQ10 “doesn’t work.” They mean it hasn’t worked reliably for everyone—or in every context—across the studies we currently have.
Could absorption be the missing piece?
Yes - very possibly.
Perhaps a better question than “Does CoQ10 work?” is “Was it absorbed?” CoQ10 is fat-soluble and absorbed through the same pathways as dietary fats. Human studies show that blood levels achieved from the same dose can differ two- to four-fold depending on formulation and if it is taken with a healthy fat to aid absorption.
What does this mean for you?
It means that two people taking “100 mg of CoQ10” may not be getting the same biological exposure at all. Solubilized, complexed, or liposomal formulations tend to result in higher and more consistent absorption than basic crystalline products.
This helps explain why:
For more detail, see:
👉 How Much CoQ10 Should I Take?
In people with chronic heart failure who are already receiving appropriate medical care, CoQ10 has the most consistent evidence for potential benefit. Even here, effects are modest and variable, but the biological rationale is strong.
For blood pressure, blood sugar, and metabolic markers, results are inconsistent. Some people see small improvements; many do not. Because positive studies may be overrepresented in the literature, these outcomes are less reliable predictors of individual benefit.
For fatigue, inflammation, and exercise performance, evidence is emerging but inconsistent. Improvements, when they occur, are often subjective and context-dependent.
Extra caution is warranted if you:
For more statin-specific information, see:
What does a fair trial look like?
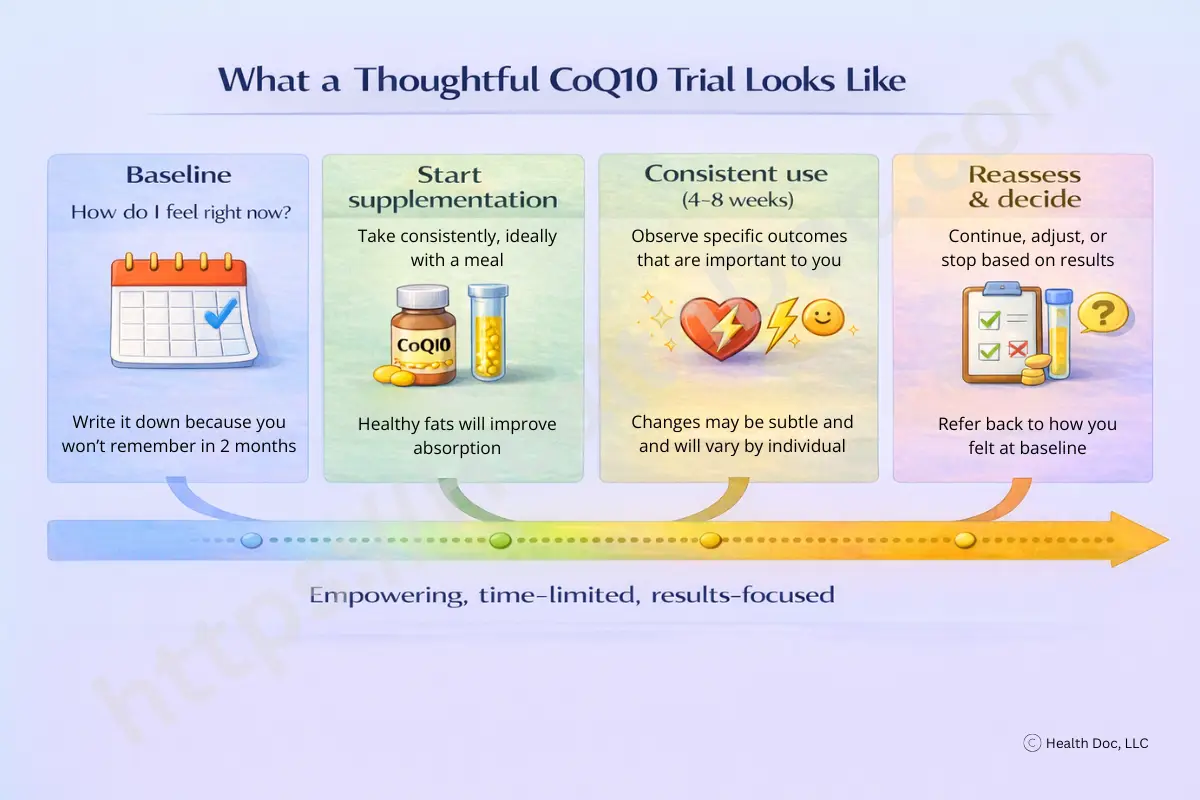
In cardiovascular research, CoQ10 doses most commonly range from ~100–300 mg/day, though optimal dosing likely varies by formulation and individual response.³
Because CoQ10 acts through mitochondrial adaptation rather than acute stimulation, weeks to months - not days - are usually required before effects, if any, are noticed.
CoQ10 is generally well tolerated, but safety is context-dependent. Case reports suggest possible interaction with warfarin, while small trials show no consistent INR change. Given warfarin’s narrow therapeutic window, clinician supervision and monitoring are advised.⁷
A “time-limited trial” doesn’t mean turning your life into an experiment.
It simply means:
In other words, treating supplementation as a test, not a lifelong commitment.
Can you support CoQ10 without supplements?
A supervised exercise-training study measuring intramuscular CoQ10 found that moderate-intensity training increased muscle CoQ10 alongside improved mitochondrial capacity, suggesting that fitter muscle simply contains more mitochondria - and more CoQ10.¹²
This does not mean exercise spikes blood CoQ10, but it reinforces the idea that mitochondrial health is shaped by lifestyle.
Sleep, stress management, and diet also influence oxidative balance and metabolic resilience, forming the foundation on which any supplement works - or fails.
CoQ10 is not a miracle supplement. It is something more interesting: a molecule at the crossroads of energy production and oxidative balance, two processes your heart relies on continuously. The science suggests that CoQ10 status reflects meaningful aspects of heart health, particularly in heart failure, but responses to supplementation vary widely.
The strongest interpretation of the evidence is not “CoQ10 works” or “CoQ10 doesn’t work,” but:
Understanding why results differ - absorption, baseline status, health context - helps move the conversation from hype to realism.
If, after consulting with your physician or healthcare provider, you decide that supplementing with coenzyme Q10 may be appropriate for you, we offer our premium CoQ10 for your consideration.
No specific CoQ10 brand has been shown to produce superior clinical outcomes across all populations, and individual responses can vary. That said, not all supplements are created equal. Differences in formulation, manufacturing standards, and quality control can meaningfully affect purity, consistency, and - importantly - absorption.
Regardless of the product you choose, look for a supplement that:
If you’d like to learn more about how we approach quality, formulation, and testing standards, you can explore our CoQ10 offering as one possible option among many.
CoQ10, or Coenzyme Q10, is a substance naturally produced by the body that helps cells generate energy. It's particularly vital for the heart due to its high energy demands.
No supplement guarantees prevention. Evidence suggests potential benefit in specific contexts, especially heart failure, but results vary.³
Not necessarily. Optimized ubiquinone formulations can match or exceed ubiquinol absorption.⁴
Yes - especially with fat, to improve absorption.⁴
Yes, particularly warfarin. Clinician guidance is recommended.⁷
You can boost CoQ10 through diet by eating foods like fatty fish, organ meats, and certain oils and nuts. Supplements are also available for those who need higher doses.
CoQ10 is generally safe with few side effects, which might include mild stomach upset. However, always consult a healthcare provider before starting any new supplement regimen.
Dosages in most clinical trials vary from 60 mg to 300 mg per day although some go higher. Your healthcare provider can help determine the best dosage for you based on your health needs.
No. While CoQ10 is generally safe, individual factors like age, lifestyle, and health status can influence its effectiveness. People with conditions affecting their heart health, those on statin medications, and individuals seeking to enhance energy levels, reduce fatigue and muscle weakness, and to improve mental acuity are the ones most likely to benefit from CoQ10 supplementation but always consult with a qualified healthcare provider before making changes to your treatment regimen.
Whether you are much interested in investing, our collection of articles is designed to educate and empower you.